ATPL brain disease is a term that has emerged in recent discussions within the medical community, generating curiosity and concern. As our understanding of neurological disorders evolves, new conditions are identified, often presenting unique challenges for diagnosis and treatment. The term "ATPL brain disease" is not yet widely recognized in mainstream medical literature, which sparks interest in understanding its implications, symptoms, and potential treatments. This article aims to provide a comprehensive overview of ATPL brain disease, offering insights into its current understanding and future directions.
The brain is a complex organ, responsible for controlling all bodily functions and processes. When a condition like ATPL brain disease arises, it can significantly impact a person's quality of life. This article is structured to guide readers through a detailed exploration of this mysterious condition, starting with its definition and potential causes. We will also delve into the symptoms, diagnostic methods, and treatment options currently available, while considering the latest research and developments in the field.
Our goal is to make this information accessible to a wide audience, including those who may be experiencing symptoms themselves or have loved ones who are affected. By shedding light on this enigmatic condition, we hope to contribute to a broader understanding and encourage further research and discussion. Whether you're a healthcare professional, a student, or someone seeking answers, this article will serve as a valuable resource on ATPL brain disease.
Table of Contents
1. What is ATPL Brain Disease?
ATPL brain disease refers to a condition that affects the brain, potentially altering its function and structure. Although it is not extensively documented in medical literature, it is believed to be a neurodegenerative disorder, which means it progressively damages nerve cells in the brain. This damage can lead to a variety of cognitive, physical, and emotional symptoms, impacting an individual's ability to perform everyday tasks.
The term "ATPL" itself is not widely recognized, leading to speculation about its origins and exact definition. It may represent a classification of symptoms or a specific pathological process, but without a clear consensus, understanding its intricacies remains challenging. As research progresses, the medical community is working to establish more concrete definitions and diagnostic criteria for ATPL brain disease.
Given the limited information currently available, it is crucial to explore potential causes and related disorders that might share similar characteristics. This exploration can offer insights into how ATPL brain disease might manifest and be managed effectively.
2. The History and Discovery of ATPL Brain Disease
The history of ATPL brain disease is relatively recent, with discussions emerging primarily in specialized medical forums and research papers. Unlike more established neurological conditions, ATPL brain disease does not have a long history of recognition or study. Its emergence can be attributed to advancements in neuroscience and the increasing ability to detect subtle changes in brain function and structure.
Initial reports of ATPL brain disease came from case studies and clinical observations, where patients presented with unusual neurological symptoms that did not fit existing diagnostic categories. These cases prompted further investigation, leading to the identification of potential patterns and commonalities among affected individuals. As more data is collected, researchers are working to piece together the puzzle of ATPL brain disease, hoping to uncover its origins and mechanisms.
The discovery of ATPL brain disease highlights the dynamic nature of medical science, where new conditions can emerge as our understanding of the human body deepens. It also underscores the importance of ongoing research and collaboration among scientists, clinicians, and patients to unravel the mysteries of such enigmatic disorders.
3. Understanding the Causes and Risk Factors
The exact causes of ATPL brain disease remain unclear, but several hypotheses have been proposed based on current research and understanding of neurological disorders. These potential causes include genetic predispositions, environmental factors, and lifestyle influences. It is likely that ATPL brain disease results from a combination of these elements, rather than a single identifiable cause.
Genetic factors may play a significant role, with some studies suggesting a hereditary component to the disease. Family history of neurological disorders could increase the likelihood of developing ATPL brain disease, although more research is needed to confirm these connections. Environmental factors, such as exposure to toxins or infections, might also contribute to the disease's onset by triggering inflammatory responses or damaging neural pathways.
Lifestyle factors, including diet, exercise, and stress levels, could influence the progression and severity of ATPL brain disease. Maintaining a healthy lifestyle may help mitigate some of the risks, although it is not a guaranteed preventive measure. Understanding these risk factors can aid in identifying individuals who may be more susceptible to the disease, enabling earlier intervention and management.
4. Signs and Symptoms of ATPL Brain Disease
The symptoms of ATPL brain disease can vary widely among individuals, making diagnosis challenging. Commonly reported symptoms include cognitive decline, such as memory loss, difficulty concentrating, and impaired judgment. These cognitive changes can significantly impact daily life, making it difficult to perform routine tasks or maintain employment.
Physical symptoms may also be present, including muscle weakness, tremors, and coordination issues. These symptoms can resemble those of other neurological disorders, such as Parkinson's disease or multiple sclerosis, further complicating the diagnostic process. Emotional and behavioral changes, such as mood swings, depression, and anxiety, are also frequently observed, adding to the complexity of the condition.
The variability in symptoms underscores the importance of comprehensive evaluation and personalized care. By recognizing the full spectrum of potential signs, healthcare professionals can better tailor treatment plans to address the unique needs of each patient, improving overall outcomes and quality of life.
5. Diagnostic Approaches in ATPL Brain Disease
Diagnosing ATPL brain disease involves a combination of clinical assessment, imaging studies, and laboratory tests. Given the lack of specific diagnostic criteria, the process often begins with a thorough evaluation of the patient's medical history and a detailed neurological examination. This initial assessment helps identify potential symptoms and rule out other conditions that might mimic ATPL brain disease.
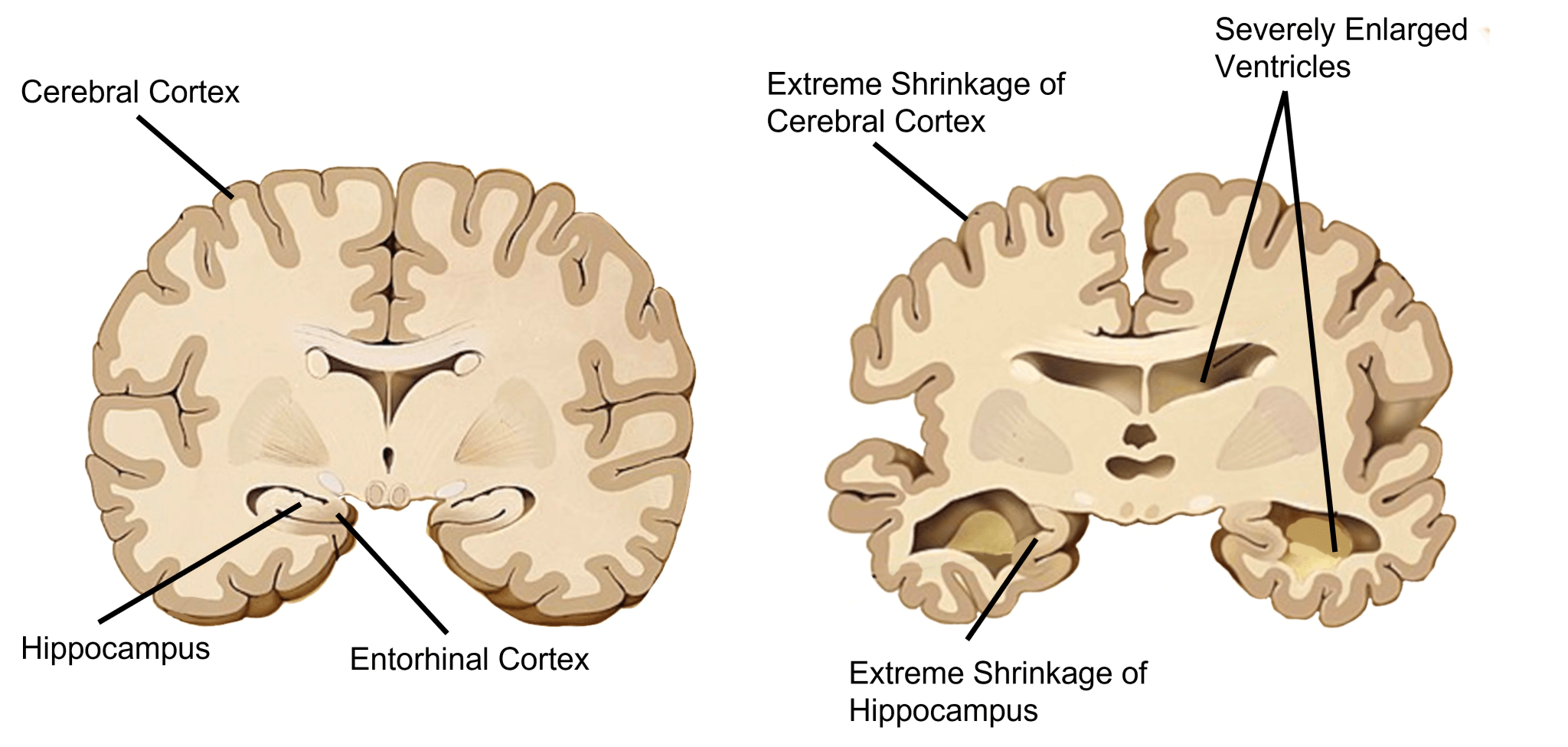
Imaging studies, such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, can provide valuable insights into structural changes in the brain. These scans may reveal abnormalities or lesions that could be indicative of ATPL brain disease, although they are not definitive on their own. Functional imaging techniques, like positron emission tomography (PET) scans, can also be used to assess brain activity and metabolism, offering further clues to the disease's presence.
Laboratory tests, including blood work and cerebrospinal fluid analysis, can help identify biochemical markers or signs of inflammation associated with ATPL brain disease. These tests are often used in conjunction with imaging studies to provide a more comprehensive picture of the patient's condition.
Ultimately, diagnosing ATPL brain disease requires a collaborative approach, involving neurologists, radiologists, and other specialists. By combining their expertise, these professionals can arrive at a more accurate diagnosis, paving the way for effective treatment and management strategies.
6. Treatment and Management Strategies
The treatment of ATPL brain disease is primarily focused on managing symptoms and improving the patient's quality of life. As there is currently no cure for the disease, medical professionals aim to alleviate its effects through a combination of pharmacological and non-pharmacological interventions.
Pharmacological treatments may include medications to address specific symptoms, such as cognitive enhancers, antidepressants, and antianxiety drugs. These medications can help improve cognitive function, stabilize mood, and reduce anxiety, although they may not be effective for all patients. Additionally, some patients may benefit from medications that target underlying inflammation or neurodegeneration, although these are still under investigation.
Non-pharmacological interventions, such as physical therapy, occupational therapy, and cognitive rehabilitation, can also play a crucial role in managing ATPL brain disease. These therapies aim to enhance physical function, improve cognitive skills, and promote overall well-being, empowering patients to maintain independence and a higher quality of life.
Support from healthcare professionals, family members, and support groups can also be invaluable in helping patients cope with the emotional and social challenges posed by ATPL brain disease. By fostering a supportive environment, patients can better navigate the complexities of their condition and maintain a sense of hope and optimism for the future.
7. The Role of Genetics in ATPL Brain Disease
Genetics may play a significant role in the development and progression of ATPL brain disease, with some evidence suggesting a hereditary component. While the specific genes involved remain unidentified, researchers are investigating potential genetic markers that could contribute to the disease's onset.
Family studies have shown that individuals with a family history of neurological disorders may be at an increased risk of developing ATPL brain disease. This observation highlights the importance of genetic counseling for those with a known family history, as it can provide valuable information about potential risks and guide decisions about preventive measures and early intervention.
Understanding the genetic basis of ATPL brain disease can also help researchers develop targeted therapies that address the underlying causes of the condition. By identifying specific genes or genetic mutations associated with the disease, scientists can work towards developing personalized treatments that improve outcomes and reduce the burden of the disease on affected individuals and their families.
8. Lifestyle Modifications and Prevention Tips
While there is no guaranteed way to prevent ATPL brain disease, certain lifestyle modifications may help reduce the risk or delay the onset of symptoms. Adopting a healthy lifestyle can support overall brain health and improve resilience against neurological disorders.
Regular physical exercise has been shown to promote brain health by increasing blood flow, reducing inflammation, and enhancing neuroplasticity. Engaging in aerobic activities, strength training, and flexibility exercises can contribute to overall well-being and may have a protective effect against ATPL brain disease.
A balanced diet, rich in fruits, vegetables, whole grains, lean proteins, and healthy fats, can also support brain health. Nutrients such as omega-3 fatty acids, antioxidants, and B vitamins have been linked to improved cognitive function and may help protect against neurodegenerative diseases.
Managing stress through relaxation techniques, such as meditation, yoga, and deep breathing exercises, can also be beneficial in maintaining mental health and reducing the risk of neurological disorders. Prioritizing sleep and ensuring adequate rest is essential for cognitive function and overall well-being.
9. Psychological and Social Impacts
ATPL brain disease can have profound psychological and social impacts on patients and their families. The emotional burden of living with a chronic, progressive condition can lead to feelings of anxiety, depression, and isolation. Patients may struggle to cope with the loss of cognitive and physical abilities, which can affect their self-esteem and overall quality of life.
Maintaining social connections and engaging in meaningful activities can help mitigate some of these emotional challenges. Support groups and counseling services can provide a safe space for patients and their families to share their experiences, learn coping strategies, and find solace in the understanding and empathy of others facing similar challenges.
Addressing the psychological and social aspects of ATPL brain disease is an essential component of comprehensive care. By fostering a supportive environment and promoting mental well-being, patients can better navigate the complexities of their condition and maintain a sense of hope and optimism for the future.
10. Recent Research and Advances
Research on ATPL brain disease is still in its early stages, but recent advances in neuroscience and technology offer promising avenues for exploration. Scientists are investigating the underlying mechanisms of the disease, including potential genetic, molecular, and environmental factors that contribute to its onset and progression.
Advancements in neuroimaging techniques, such as functional MRI and PET scans, have improved our ability to visualize and study changes in brain structure and function associated with ATPL brain disease. These tools enable researchers to identify potential biomarkers and develop more accurate diagnostic criteria, paving the way for earlier intervention and more effective treatments.
Emerging therapies, such as gene editing, stem cell therapy, and neuroprotective agents, are being explored as potential treatments for ATPL brain disease. While these approaches are still in the experimental stages, they hold promise for addressing the underlying causes of the disease and improving patient outcomes in the future.
11. Case Studies and Patient Stories
Case studies and patient stories provide valuable insights into the lived experiences of individuals with ATPL brain disease. By sharing their journeys, patients and their families can offer unique perspectives on the challenges and triumphs associated with the condition.
These narratives can highlight the importance of early diagnosis, personalized care, and the power of resilience in the face of adversity. They also underscore the need for continued research and advocacy to raise awareness and improve resources for those affected by ATPL brain disease.
By learning from the experiences of others, patients and their families can gain a better understanding of the condition and find inspiration and support in their own journeys. These stories serve as a testament to the strength and determination of those living with ATPL brain disease and their commitment to overcoming its challenges.
12. Support and Resources for Patients and Families
Access to support and resources is crucial for patients and families affected by ATPL brain disease. Navigating the complexities of the condition can be overwhelming, but a strong support network can provide invaluable assistance and guidance.
Healthcare professionals, including neurologists, therapists, and social workers, can offer expert advice and support for managing symptoms and improving quality of life. Support groups and online communities can connect patients and families with others facing similar challenges, fostering a sense of camaraderie and understanding.
Educational resources, such as books, articles, and websites, can provide valuable information about ATPL brain disease, helping patients and families make informed decisions about their care. Advocacy organizations can also offer resources and support for navigating the healthcare system and accessing necessary services.
13. Frequently Asked Questions (FAQs)
What is ATPL brain disease?
ATPL brain disease is a neurodegenerative condition that affects the brain, leading to cognitive, physical, and emotional symptoms. Although not widely recognized in mainstream medical literature, it is believed to share characteristics with other neurological disorders.
How is ATPL brain disease diagnosed?
Diagnosis involves a combination of clinical assessment, imaging studies, and laboratory tests. A thorough evaluation of the patient's medical history, neurological examination, and various imaging techniques help identify potential symptoms and rule out other conditions.
What are the symptoms of ATPL brain disease?
Common symptoms include cognitive decline, such as memory loss and impaired judgment, physical symptoms like muscle weakness and tremors, and emotional changes such as mood swings, depression, and anxiety.
Is there a cure for ATPL brain disease?
Currently, there is no cure for ATPL brain disease. Treatment focuses on managing symptoms and improving the patient's quality of life through a combination of pharmacological and non-pharmacological interventions.
What role does genetics play in ATPL brain disease?
Genetics may play a significant role in the development and progression of ATPL brain disease, with some evidence suggesting a hereditary component. Ongoing research aims to identify specific genetic markers associated with the condition.
How can lifestyle modifications help with ATPL brain disease?
Adopting a healthy lifestyle, including regular exercise, a balanced diet, stress management, and adequate sleep, may help reduce the risk or delay the onset of symptoms, although it is not a guaranteed preventive measure.
14. Conclusion and Future Outlook
ATPL brain disease remains a relatively enigmatic condition, but ongoing research and advances in neuroscience offer hope for a better understanding and improved management of the disease. As our knowledge of the brain continues to grow, so too does our ability to identify and address previously unrecognized disorders.
By fostering collaboration among researchers, healthcare professionals, patients, and their families, we can work towards developing more effective diagnostic tools, treatments, and support resources for those affected by ATPL brain disease. As awareness of this condition increases, so too does the potential for positive change and improved outcomes for patients and their loved ones.
The journey towards understanding ATPL brain disease is just beginning, but with continued dedication and perseverance, we can look forward to a future where those affected by this condition can lead healthier, happier lives.
For more information on related neurological disorders and ongoing research, visit the National Institute of Neurological Disorders and Stroke: NINDS.
Article Recommendations

ncG1vNJzZmiclaK8b7HNnqmgoaOirrPAjaemaKaVrMCis8SnmrJpZWSutbzLZpmrmZmjeqW10p6YrJ1encGuuA%3D%3D